She was again in a confusional state (delirium) of unknown cause, probably recurrent infection.
Of note, almost every time I see hospital EHRs, I note a problem.
In my Jan. 2011 post on this issue at the same organization, "EHR Problems? No, They're Merely Anecodotal; the Truth Must Be That I Attract Bad Electrons and Stale Bits" I observed a nurse-stated "glitchy-ness" that day that manifested as unreliability in pulling up the patients' current med lists. I had to be the conduit of my mother's meds, despite having gone through them in detail for computer entry in the exact same ED just 24 hours prior after a fall:
This was not the "FirstNet" ED EHR by Cerner forensically analyzed by Dr. Jon Patrick (as I wrote about here), but another ED EHR, by a company whose ICU physiological monitoring system I once as CMIO struggled with due to repeated, unexplained crashing.
On this most recent ED visit/admission to the satellite just days ago, I noted another problem with the ED EHR system (the same one that started my mother's travails at the main facility in May 2010, and now in use at the satellite).
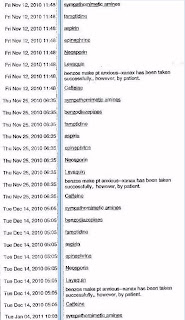
When the ED nurse brought up my mother's allergies, they were repeated over and over and over on the ED screen, in a long recurrent list dozens of lines long, as if they'd been cut-and-pasted multiple times at each visit. She apologized to me. See images of a printout that was provided to me by an ED attendant upon my request as my mother's POA, below (names of hospital, patient, EHR, and EHR screen layout digitally redacted):
Note that on-screen these appeared as a long, confusing list.
The repetition made the list near useless to the ED personnel (for example, they don't have time to look for the one crucial item that ISN'T a duplicate in the mess).
Legible gibberish indeed.
The ED RN just asked me about my mother's allergies, saying she could not make sense of the computer list and wanted to make sure no mistakes occurred. This is an appropriate attitude - the only appropriate attitude - for a clinician. Fortunately, I'm a doctor and know the allergies well.
The hospitalist then called me that night suggesting she would give my mother Levaquin, an antibiotic. For the umpteenth time I had to tell a doctor at these facilities my mother was allergic to Levaquin. This was in fact one of my complaints on my April 2010 warning letter to the hospital's CEO and CMO on EHR deficiencies I'd noted in my mother's care. This was just one month prior to her catastrophe, when a critical heart medication "disappeared" in the ED EHR, causing a cascade of medication continuity failure.
Yesterday I insisted the duplicate entries be removed (more precisely, "made inactive" - they still appear, but in a different color than "active" entries).
It is, on first principles, inherently harmful to the public to have critical patient data stored in disarray in an Emergency Room electronic health record.
See the above images, and ask if this is what you'd want busy ED doctors to have to wade through to figure out if a drug they're about to administer might injure or kill you.
-- SS
Post legal-threat addendum:
I'd originally posted actual screen shots (PHI and hospital name redacted) of the allergy lists provided to me by an ED attendant upon my request as my mother's POA.
On April 8, 2011, however, I received a threatening letter from the attorney representing the hospital claiming these screens were viewed by the client as "copyrighted and proprietary information" that I had "misappropriated" (stolen).
(This raises the question as to who, exactly, the "client" is - the hospital, or the EHR vendor?)
In any case, I was asked to "retract from the blog the copyrighted and proprietary information" under threat of the hospital "pursuing all remedies under the state's trade secret laws and Federal Law." Further, I was accused of "inappropriate behavior" in trying to protect my mother from further EHR-related accidents.
The allegations (actually, fabrications) of "medical records misappropriation" and "inappropriate behavior" were especially outrageous and unprofessional, considering the hospital had already altered my mother's medical record by adding the medication they missed to the ICU H&P as at this post, was caught at it, and had admitted it to me.
I have now done as asked, only posting the allergy information and dates without the background EHR tabs of the screen header, the only component that could even remotely be viewed as protected IP (i.e., of the EHR vendor).
I had a followup discussion with a senior nurse involved in the EMR project about those screens and the legal threats, which I viewed as potential retaliation aimed at discriminatorily denying my mother and I use of public accommodations, i.e., the hospital, through intimidation. (If my seeking records legitimately was "inappropriate behavior", who knew what else I might be falsely accused of to "discourage" my return?)
I was informed with a straight face that the allergy repetition was a "feature", not a bug.
The problem was "the nurse in the ED", who did not understand they needed to "look at the dates" to understand the allergy list. ["Blame the user" is typical in this domain - ed.] This senior nurse clearly had an amateur's understanding of HCI and clarity of presentation of information - or was simply talking down to me.
I provided a reminder that with 20 years of Ivy academic, big hospital (much larger than hers) and Big Pharma experience in this domain, I found her arguments specious.
Amateurism on presentation of information is a factor that promotes EHR-related error. (It is my hope the original ED nurse is not punished for protecting patients instead of "protecting the computer" and its faults.)
-- SS
In my Jan. 2011 post on this issue at the same organization, "EHR Problems? No, They're Merely Anecodotal; the Truth Must Be That I Attract Bad Electrons and Stale Bits" I observed a nurse-stated "glitchy-ness" that day that manifested as unreliability in pulling up the patients' current med lists. I had to be the conduit of my mother's meds, despite having gone through them in detail for computer entry in the exact same ED just 24 hours prior after a fall:
... My mother was having a repeat of the ischemia to the brain or "TIA" (transient ischemic attack, i.e., threatening to have a stroke), only this time the ED EHR itself was also having a TIA.
This was not the "FirstNet" ED EHR by Cerner forensically analyzed by Dr. Jon Patrick (as I wrote about here), but another ED EHR, by a company whose ICU physiological monitoring system I once as CMIO struggled with due to repeated, unexplained crashing.
On this most recent ED visit/admission to the satellite just days ago, I noted another problem with the ED EHR system (the same one that started my mother's travails at the main facility in May 2010, and now in use at the satellite).
When the ED nurse brought up my mother's allergies, they were repeated over and over and over on the ED screen, in a long recurrent list dozens of lines long, as if they'd been cut-and-pasted multiple times at each visit. She apologized to me. See images of a printout that was provided to me by an ED attendant upon my request as my mother's POA, below (names of hospital, patient, EHR, and EHR screen layout digitally redacted):
Note that on-screen these appeared as a long, confusing list.
The repetition made the list near useless to the ED personnel (for example, they don't have time to look for the one crucial item that ISN'T a duplicate in the mess).
Legible gibberish indeed.
The ED RN just asked me about my mother's allergies, saying she could not make sense of the computer list and wanted to make sure no mistakes occurred. This is an appropriate attitude - the only appropriate attitude - for a clinician. Fortunately, I'm a doctor and know the allergies well.
The hospitalist then called me that night suggesting she would give my mother Levaquin, an antibiotic. For the umpteenth time I had to tell a doctor at these facilities my mother was allergic to Levaquin. This was in fact one of my complaints on my April 2010 warning letter to the hospital's CEO and CMO on EHR deficiencies I'd noted in my mother's care. This was just one month prior to her catastrophe, when a critical heart medication "disappeared" in the ED EHR, causing a cascade of medication continuity failure.
Yesterday I insisted the duplicate entries be removed (more precisely, "made inactive" - they still appear, but in a different color than "active" entries).
It is, on first principles, inherently harmful to the public to have critical patient data stored in disarray in an Emergency Room electronic health record.
See the above images, and ask if this is what you'd want busy ED doctors to have to wade through to figure out if a drug they're about to administer might injure or kill you.
-- SS
Post legal-threat addendum:
I'd originally posted actual screen shots (PHI and hospital name redacted) of the allergy lists provided to me by an ED attendant upon my request as my mother's POA.
On April 8, 2011, however, I received a threatening letter from the attorney representing the hospital claiming these screens were viewed by the client as "copyrighted and proprietary information" that I had "misappropriated" (stolen).
(This raises the question as to who, exactly, the "client" is - the hospital, or the EHR vendor?)
In any case, I was asked to "retract from the blog the copyrighted and proprietary information" under threat of the hospital "pursuing all remedies under the state's trade secret laws and Federal Law." Further, I was accused of "inappropriate behavior" in trying to protect my mother from further EHR-related accidents.
The allegations (actually, fabrications) of "medical records misappropriation" and "inappropriate behavior" were especially outrageous and unprofessional, considering the hospital had already altered my mother's medical record by adding the medication they missed to the ICU H&P as at this post, was caught at it, and had admitted it to me.
I have now done as asked, only posting the allergy information and dates without the background EHR tabs of the screen header, the only component that could even remotely be viewed as protected IP (i.e., of the EHR vendor).
I had a followup discussion with a senior nurse involved in the EMR project about those screens and the legal threats, which I viewed as potential retaliation aimed at discriminatorily denying my mother and I use of public accommodations, i.e., the hospital, through intimidation. (If my seeking records legitimately was "inappropriate behavior", who knew what else I might be falsely accused of to "discourage" my return?)
I was informed with a straight face that the allergy repetition was a "feature", not a bug.
The problem was "the nurse in the ED", who did not understand they needed to "look at the dates" to understand the allergy list. ["Blame the user" is typical in this domain - ed.] This senior nurse clearly had an amateur's understanding of HCI and clarity of presentation of information - or was simply talking down to me.
I provided a reminder that with 20 years of Ivy academic, big hospital (much larger than hers) and Big Pharma experience in this domain, I found her arguments specious.
Amateurism on presentation of information is a factor that promotes EHR-related error. (It is my hope the original ED nurse is not punished for protecting patients instead of "protecting the computer" and its faults.)
-- SS


I can not determine what is worse, the defective equipment, or that the doctors see chit and put up with this crap.
ReplyDeleteScot, Do you think that perhaps they are purposfully not listing Levaquin as something she is allergic to because if they did, their liability in prior events would be easier to prove?
ReplyDeleteIn other words, the EHR is not intended to help the patient, it is intended to help the hospital lawyers and protect the adminsitrator's profit?
Live IT or live with it said...
ReplyDeleteperhaps they are purposfully not listing Levaquin
Levaquin is listed.
Over and over and over. See printout sheets.
Busy physicians and nurses have to wade through crap like this, which appears even more crowded and confusing on-screen, and requires scrolling, screen navigation, etc. besides.
I would like someone - anyone - to tell me how that aids the safe practice of medicine. Any takers?
The intake nurse simply asked me about my mother's allergies, apologizing to me personally that the ED list was in this "repetitive" disarray.
-- SS
I don't know if "Other, z_undef" is admitting to knowing an allergy exists. Could be though that I misunderstand the terminology of the list (imagine that?).
ReplyDeleteI mean the whole idea of a "Known Medication" list being filled with so many Unknowns and Undefineds is on its face unfathomable.
ReplyDeleteOf course none of that matters since you are violating HIPAA by including the discharge date. The first line of HIPAA defense if the Hospital's Privacy Officer. Their "Privacy Officer" is not first bound to protect patients but rather they are first charged with reducing the hospital's legal liability (most hospital privacy officers are also their lawyers).
They may be writing you a tome soon.
I didn't even get into the issue of why the details of each allergy are largely meaningless.
ReplyDeleteTo fill them in would require time to actually ask the patient and/or family. This organization seems to have deemed that information of no value, as I've offered the details many times, but it never seems to make it into the electronic record.
-- SS
Anonymous March 22, 2011 11:19:00 PM EDT writes:
ReplyDeleteOf course none of that matters since you are violating HIPAA by including the discharge date ... They may be writing you a tome soon.
I will publish it here if it appears.
-- SS
Great post -- thanks for fighting this fight.
ReplyDelete